Every state is struggling with the explosive growth and cost of its Medicaid program. That will be doubly true in a few years for the states that have accepted the Affordable Care Act’s Medicaid expansion because the federal government will soon stop paying 100 percent of the costs. However, Illinois and Pennsylvania found a way to reduce their Medicaid spending significantly, freeing up money for other important projects—or better yet, tax cuts. And other states should join them.
Medicaid’s Growth Binge
Medicaid is the federal-state health insurance program for the poor and disabled. The Department of Health and Human Services (HHS) estimates that Medicaid covered 72.2 million people for at least one month in 2012.1
However, Medicaid enrollment is growing quickly. The Centers for Medicare and Medicaid Services (CMS) reports that Medicaid and the state Children’s Health Insurance Program (CHIP) enrollment is up by about 8.7 million people, nearly 15 percent, since the ACA’s October 2013 rollout.2 Medicaid expansion states are seeing an average enrollment growth of 22 percent, and 10 of those states are experiencing 30 percent growth, according to CMS. The non-expansion states are also seeing growth in Medicaid, but only about 5 percent.3
Historical and Projected Medicaid Enrollment and Annual Growth Rates, FY 1966- FY 2022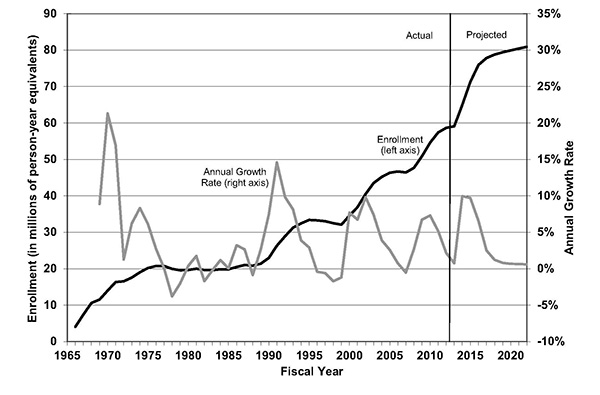
Medicaid’s Spending Binge
Total Medicaid spending was about $432 billion in 2012, with the federal government providing $250 billion, or 58 percent, and states funding the rest.4
For many states Medicaid is their largest budget item, and virtually all are struggling to cover their costs, forcing them to limit or reduce spending in other important areas like education and welfare in order to pay their Medicaid bills.
But Medicaid is a government-run health insurance program and is plagued with the problems of inefficiency, waste, rampant fraud, and lack of timely access to quality care. Just think of the recent Veterans Administration scandal, only worse. States are looking for solutions and two states found one.
Case Study: Illinois
As Illinois entered its 2013 fiscal year, the Medicaid budget faced a shortfall of $2.7 billion. The state had begun implementing some of the reforms that other states are incorporating, such as shifting more Medicaid recipients into private sector Medicaid managed care organizations (MCOs), but it needed to find even more savings.
In response, Illinois state Representative Patti Bellock garnered bipartisan support to pass the SMART Act in 2012, which included several Medicaid reforms. One of the most important of those was a provision to establish the Illinois Medicaid Redetermination Program (IMRP) to "redetermine" if Medicaid enrollees were still eligible to participate.
The federal government requires states to do an annual audit of the Medicaid rolls to ensure that all enrollees are eligible, but in most states few people are actually removed. Bellock wanted to use an outside, private sector firm, Virginia-based Maximus, to audit the state’s 1.3 million Medicaid case files—which represents about 2.7 million individuals. The company has more extensive databases than the state and would likely identify more ineligible Medicaid beneficiaries.
And it did just that. Maximus recommended removing 249,912 cases by the end of February 2014, according to the state.5 By law a state employee has to review the recommendations and decide if cancellation is appropriate. The state removed 148,283 cases (representing 234,000 individuals) from the Medicaid rolls.
However, the American Federation of State, County and Municipal Employees (AFSCME) filed suit claiming that most of the work should be done by state bureaucrats, and a federal judge agreed. Although the outside vendor is still involved, it’s role has been reduced significantly. Even so, the state has continued to identify people who should be dropped from the Medicaid rolls. According to state data, 173,469 Medicaid cases have been cancelled between February and September.6
Not all of these cancellations are the result of fraud. Many simply did not respond to the state’s repeated inquiries. Or a Medicaid beneficiary might get a job or a raise or coverage through a spouse and is no longer eligible for Medicaid but doesn’t notify the state. Or the beneficiary moves out of state without realizing that Medicaid is a state-based plan. And the Illinois audit found that more than 8,000 dead people were still on the state’s Medicaid rolls.
The state has struggled to determine how much money the redetermination process has saved because Medicaid covers different populations with vastly different health care costs. For example, the Kaiser Family Foundation estimates that Illinois children cost about $2,630 per year (2010), while their mothers cost $3,717—those groups make up the large majority of Medicaid beneficiaries.7 Disabled and long-term care recipients are much more costly. Canceling thousands of cases saves a lot of federal and state taxpayer money.
Case Study: Pennsylvania
The Keystone State also cut its rolls, but with a somewhat different approach. After introducing several Medicaid cost-saving measures as Rhode Island’s secretary of Health and Human Services, Gary Alexander went to Pennsylvania as secretary of the Department of Public Welfare to tackle both Medicaid and welfare.
In July 2011, the Pennsylvania legislature passed broad legislation intended to weed out waste, fraud and abuse in the state’s welfare system to get welfare spending under control. Rather than turning to an outside group, Alexander hired someone to manage his Enterprise Wide Program Integrity Initiative to ensure that people on the welfare rolls, including Medicaid, were actually eligible for the program. Within 18 months some 220,000 people were removed from the welfare rolls, saving the state about $710 million, according to Alexander.
A former state Medicaid director says Alexander, whose initiative won an innovation award from the Council of State Governments, took the right approach because Medicaid is so intertwined with the other welfare programs.
The Never-Ending Story
The redetermination process is not a one-shot effort. Every day thousands of people become eligible for Medicaid, and thousands no longer are. That process will be exacerbated by the president’s Medicaid expansion. For example, nearly 477,000 adults newly eligible for Medicaid under the ACA have already signed up, a number that is sure to grow in the future.
Conclusion
While Pennsylvania focused on its broader welfare population, Illinois directed its redetermination efforts primarily at the Medicaid program. Both efforts succeeded, though the Illinois redetermination program received bipartisan support, while there were numerous critics of the Pennsylvania effort.
States are facing serious Medicaid budget challenges and many need to address the problem quickly. A redetermination program is a good start. Fighting waste and fraud can be a bipartisan battle. Getting ineligible beneficiaries off the rolls allows the state to use that money for other purposes—or return it to the taxpayers.
Endnotes
3. Ibid.
6. Department of Human Services, "Medicaid Redetermination Data," Oct. 9, 2014.
7. Henry J. Kaiser Family Foundation, "Medicaid Payments Per Enrollee."
